The basics of Transcranial Magnetic Stimulation (TMS)
Transcranial Magnetic Stimulation (TMS) is a medical device which applies electrical pulses to the brain using a magnetic coil held over the head. An electric current is delivered to the coil by a stimulator, and the current flowering through loops in the coil generates a magnetic field. The magnetic field goes through the head (skull) to the brain where it produces an electrical stimulation of the brain. A specific pattern (waveform) of current is applied to the coil which is replicated in the brain; the right pattern can change brain function and be used to treat neurological and psychiatric disorders, such as depression.
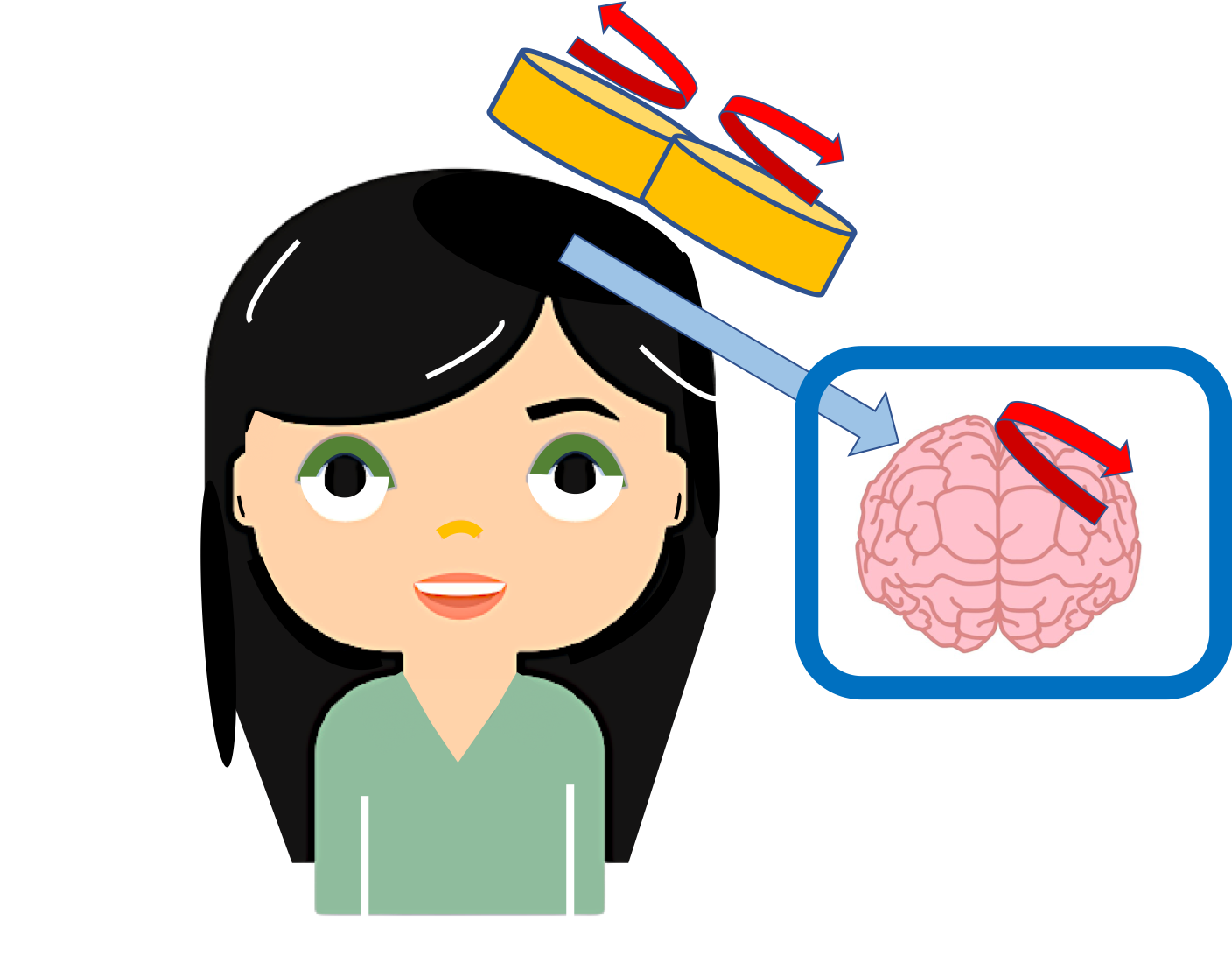
There is a lot of current produced by the stimulator into the coil, and this leads to a significant amount of electricity being produced in the brain. The coil produced by the stimulator does not directly go into the person, it only goes into the coil. The electricity produced in a person's head is a lot less than that in the coil and is transmitted through the skull to the brain through a magnetic field. Hence it is called “transcranial” “magnetic” stimulation.
If the coil is positioned over the part of the brain involved in motion, then when the Transcranial Magnetic Stimulation (TMS) is turned on, an involuntary muscle twitch is produced. For example, a finger twitch This is not dangerous and only mildly uncomfortable. In fact, the TMS muscle twitch is typically used in TMS therapy of diseases as part of calibrating the device for each person’s head.
When Transcranial Magnetic Stimulation (TMS) is used to produce a motor twitch, just a single quick pulse of current is sent to the coil. When TMS is used to treat depression or other neuropsychiatric disorders, a train of pulses is applied – on after the other. These pulses come quickly one after the other, so “repeatedly”. For this reason, when TMS is used for treatment it is called repeated Transcranial Magnetic Stimulation or rTMS. rTMS is a type of TMS and the terms are sometimes used interchangeably when talking about TMS therapy. A session of rTMS can last 30 to 60 minutes, only part of that time is TMS being applied and the rest of the time is used for set-up.
During the TMS procedure, the subject sits in a comfortable chair, usually with a head rest. A doctor or medical technician will position the coil over the subject’s head and program the right pulse waveform into the device. The sensation isn’t typically painful and can feel like tapping on the head or little tingly shocks or muscle twitches. The sensation goes away as soon as the TMS is stopped. If you should get TMS and what kind of side-effects you might expect is something that must be discussed with your doctor, and some people report more serious side-effects like headache. Though rare, rTMS does come with a small risk of seizures.
rTMS is FDA approved for the treatment of some kinds of severe Depression. Some types of TMS are approved for treatment of certain forms of pain (such as Migraine) or obsessive-compulsive disorder (OCD). Some other applications TMS is tested for include stroke rehabilitation, Parkinson’s, depression, migraine, pain management, and auditory hallucination. Patients are attracted to rTMS because it is a non-drug therapy that has been shown to work in some patients who do not reflect well on traditional drug therapy. rTMS can be only obtained at a hospital or clinic through a certified rTMS provider.
SUMMARY
- Transcranial Magnetic Stimulation (TMS) is a medical device which applies electrical pulses to the brain using a magnetic coil held over the head.
- During the TMS procedure, the subject sits in a comfortable chair, usually with a head rest. A doctor or medical technician will position the coil over the subject’s head and program the right pulse waveform into the device
- rTMS is FDA approved for the treatment of some kinds of severe Depression
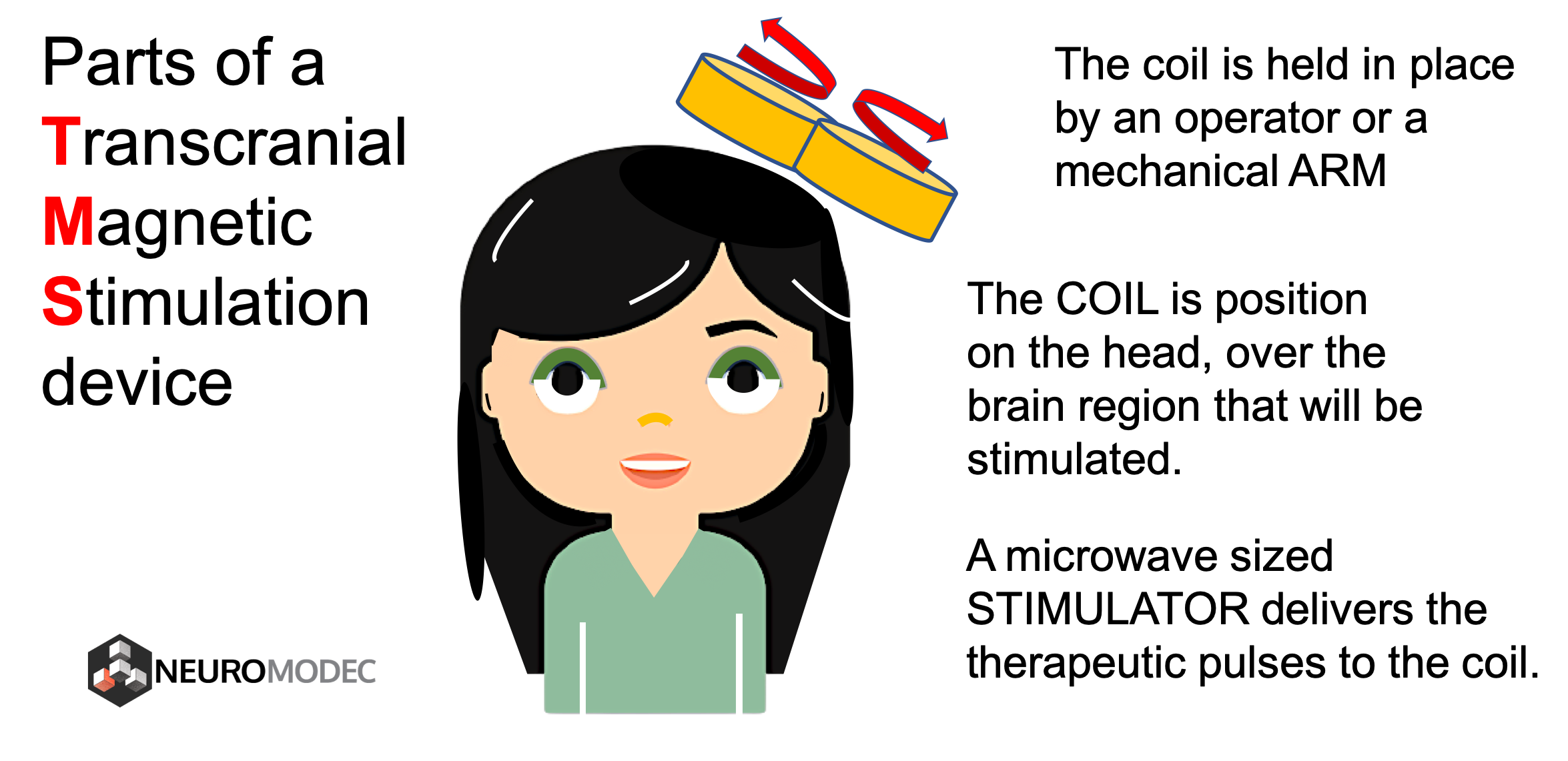
What does a TMS device look like?
A TMS stimulator is the size of mini-fridge and has a power cable. It will have various controls on it to adjust stimulation parameters such as pulse intensity, number of pulses, and pulse frequency. The coil looks like one or more loops. For example, a “figure-8 coil” is two touching loops. A cable connects the coil to the stimulator. The coil is held over the head (the part to be stimulated) by the hand of the operator, or by a mechanical arm.
What does TMS feel like? What are the side-effects?
Repetitive TMS is a noninvasive form of brain stimulation used for depression. Unlike vagus nerve stimulation or deep brain stimulation, rTMS does not require surgery or implantation of electrodes. And, unlike electroconvulsive therapy (ECT), rTMS doesn’t cause seizures or require sedation with anesthesia. According to Mayo Clinic2, rTMS is generally considered safe and well-tolerated. However, it can cause some side effects. Common side-effects effects of TMS stimulation are related to discomfort on the scalp. This discomfort should go away after the TMS session. Rarely, someone might faint or have a seizure while undergoing stimulation. Other potential side effects include: a transient confusion related to disruptions in cognition, hearing, or vision.
Common side effects:
Side effects are generally mild to moderate and improve shortly after an individual session and decrease over time with additional sessions. According to Mayo Clinic, side effects may include:- Headache
- Scalp discomfort at the site of stimulation
- Tingling, spasms or twitching of facial muscles
- Lightheadedness
Your doctor can adjust the level of stimulation to reduce symptoms or may recommend that you take an over-the-counter pain medication before the procedure.
Uncommon side effects
Serious side effects are rare. According to Mayo Clinic, uncommon side effects may include:- Seizures
- Mania, particularly in people with bipolar disorder
- Hearing loss if there is inadequate ear protection during treatment
More study is needed to determine whether rTMS may have any long-term side effects.
Where can I get TMS?
In the United State rTMS has been approved by the FDA for the treatment of some kinds of depression. You can use this free tool to find doctors and clinics who provide TMS treatment.
What is the science behind TMS?

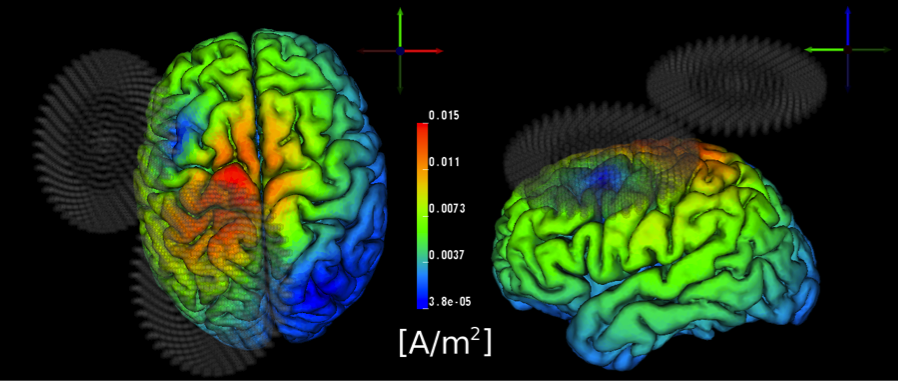
TMS is a neuromodulatory technique which applies magnetic pulses to the brain via a ‘coil.’ An electric current is delivered to the coil, which acts as the magnetic field generator in the procedure. The generated magnetic field induces an electrical current in the brain. Different coil types are used to elicit different magnetic field patterns, and using more focal points can elicit a deeper magnetic field to stimulate deeper cortical layers. Stimulation is typically applied at a sufficient intensity to trigger action potentials in proximate neurons. For example, TMS over the motor cortex can result in a finger twitch. Applying several pulses of TMS in a row is called repetitive TMS or “rTMS.” The timing of the pulses can determine how the brain changes in response. rTMS can sometimes disrupt how a brain region is working, leading to what is called a “functional lesion.” This selective interference gives it credence in therapies aiming to modulate the relative excitability of a brain region. Additionally, when combined with other neuroimaging techniques, TMS can be used to map behavior related circuitry with spatial and temporal precision1 rTMS can lead to lasting changes in brain function which is why it is used for treatment. Long-term potentiation (LTP) and long-term depression (LTD) are the implicated cellular mechanisms behind rTMS. Some areas TMS is currently being explored include: stroke rehabilitation, parkinson’s, depression, migraine, pain management, and auditory hallucination.
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
References
1. Siebner, H. R., Bergmann, T. O., Bestmann, S., Massimini, M., Johansen-Berg, H., Mochizuki, H., … & Pascual-Leone, A. (2009). Consensus paper: combining transcranial stimulation with neuroimaging. Brain stimulation, 2(2), 58-80. 2. Mayo Clinic Staff. (2018, November 27). Transcranial magnetic stimulation. Retrieved February 4, 2019, from https://www.mayoclinic.org/tests-procedures/transcranial-magnetic-stimulation/about/pac-20384625

