Overview of Spinal Cord Stimulation
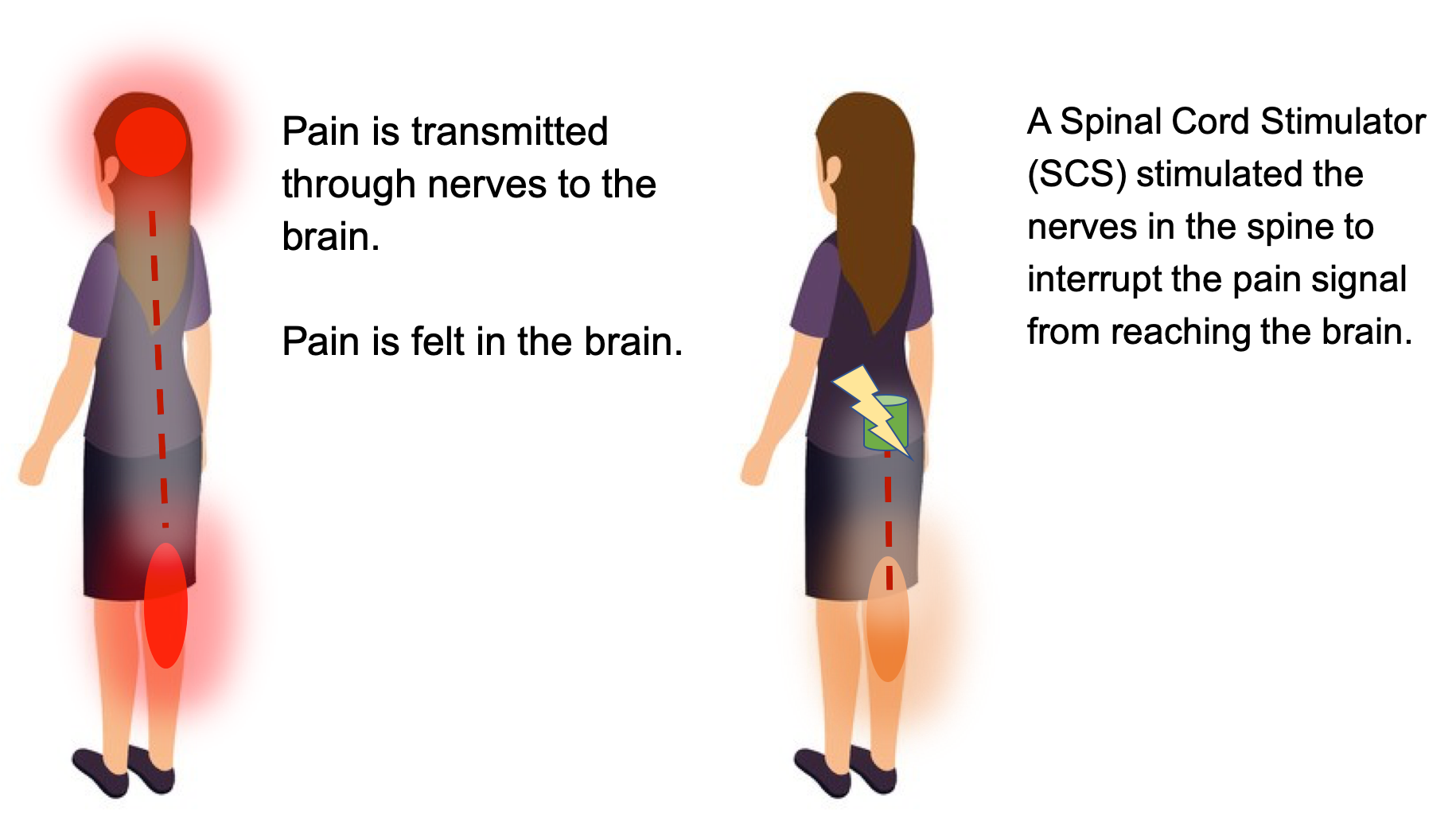
Spinal cord stimulation is a therapy that masks pain signals before they reach the brain. A small device, similar to a pacemaker, is implanted in the body to deliver electrical pulses to the spinal cord. It helps people better manage their chronic pain symptoms and decrease the use of opioid medications. It may be an option if you suffer chronic back, leg or arm pain and have not found relief with other therapies.
What is a Spinal Cord Stimulator?
A spinal cord stimulator (SCS) device is surgically placed under your skin and sends a mild electric current to your spinal cord (Fig. 1). The spinal cord device consists of a pulse generator, a small wire that carries the current from a pulse generator to the nerve fibers of the spinal cord. When turned on, the SCS stimulates the nerves in the area where your pain is felt. Pain is reduced when the electrical pulses modify and mask the pain signal from reaching your brain.
Who is a candidate for Spinal Cord Stimulation (SCS)?
Patients who are selected for Spinal Cord Stimulation (SCS) usually have had chronic debilitating pain for several months in the lower back, leg, or arm. Other therapies have not worked well enough for these patients. They also often have had one or more spinal surgeries. An evaluation of your physical condition, medication regime, and pain history by a doctor will determine whether your goals of pain management are appropriate for Spinal Cord Stimulation (SCS). A neurosurgeon, physiatrist, or pain specialist will review all previous treatments and surgeries. There may be exclusion factors for SCS or risk factors that you doctor will consider and discuss with you.
An SCS can help lessen chronic pain caused by:
- Chronic leg (sciatica) or arm pain: ongoing, persistent pain caused by arthritis, spinal stenosis, or by nerve damage.
- Failed back surgery syndrome: failure of one or more surgeries to relieve persistent arm or leg pain, but not a technical failure of the original procedure.
- Complex regional pain syndrome: a progressive disease in which patients feel constant, chronic burning pain, typically in the foot or hand.
- Arachnoiditis: painful inflammation and scarring of the protective lining of the spinal nerves.
- Other: stump pain, angina, peripheral vascular disease, multiple sclerosis, or spinal cord injury.
SUMMARY
- Spinal cord stimulation is a therapy that masks pain signals before they reach the brain. It may be an option if you suffer chronic back, leg or arm pain and have not found relief with other therapies.
- The spinal cord device consists of a pulse generator, a small wire that carries the current from a pulse generator to the nerve fibers of the spinal cord.
- Patients who are selected for Spinal Cord Stimulation (SCS) usually have had chronic debilitating pain for several months in the lower back, leg, or arm. Other therapies have not worked well enough for these patients.
What does Spinal Cord Stimulation (SCS) feel like?
Stimulation does not eliminate the source of pain, instead it interferes with the pain signal reaching the brain, which is where you feel pain. The amount of pain relief varies for each person. Spinal Cord Stimulation may produce a tingling sensation, usually over the part of the body that hurts.
What is Spinal Cord Stimulation (SCS) parasthesia?
Because Spinal Cord Stimulation (SCS) works by interrupting nerve carrying pain signals to the brain, SCS can also produce tingling over these painful areas called “paresthesia”.
Some SCS devices will usually replace the pain sensation with a mild tingling feeling called paresthesia. Other SCS devices are able to mask the pain with no tingling feeling. A paresthesia-free setting is an option on some devices and works for some patients.
Does Spinal Cord Stimulation (SCS) work for everyone?
Stimulation does not work for everyone. Some patients may find the sensation unpleasant. In other cases it may not cover the entire pain area. For these reasons a trial stimulation is performed before the device is permanently implanted. If unsuccessful, the trial wires can be removed, leaving no damage to the spinal cord or nerves.
What are the parts of a Spinal Cord Stimulation (SCS) device?
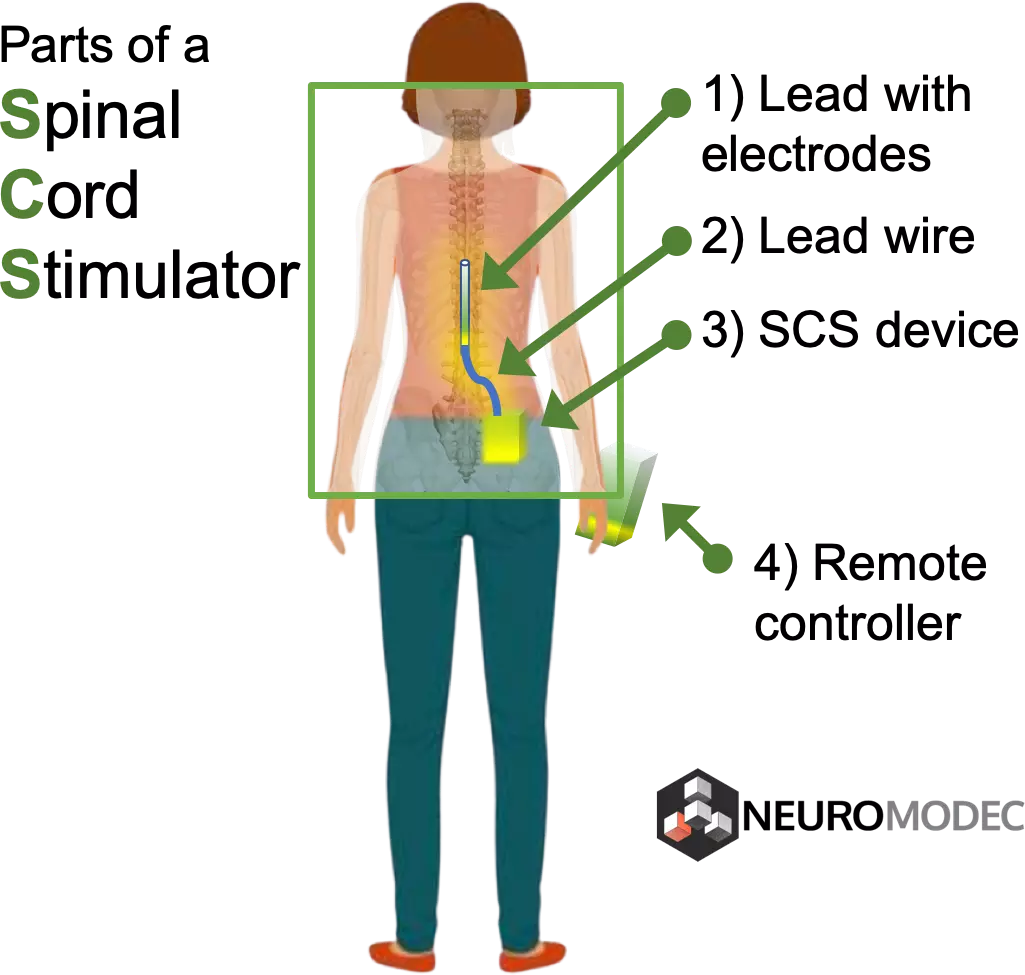
There are several types of SCS device systems. However, all have three main parts:
- A pulse generator with a battery that creates the electrical pulses.
- A lead wire with a number of electrodes (8-32) that delivers electrical pulses to the spinal cord.
- A hand-held remote control that turns the device on and off and adjusts the settings.
What is the difference between a rechargeable and non-rechargeable Spinal Cord Stimulation (SCS) device?
Systems with a non-rechargeable battery need to be surgically replaced every 2 to 5 years, depending on the frequency of use. Rechargeable battery systems may last 8 to 10 years or longer, but you must remember to charge the system daily.
The pulse generator has programmable settings. Some SCS devices are able to sense a change in body position (sitting vs. lying down) and adapt the stimulation level to your activity. Other systems have leads that can be independently programmed to cover multiple pain areas. Some send a sub-perception pulse with no tingling. Your doctor will select the best type of system for you.
Who performs the procedure for Spinal Cord Stimulation?
Neurosurgeons and doctors who specialize in pain management (an anesthesiologist or physiatrist) implant spinal cord stimulators. You can use this free tool to find doctors and clinics who provide SCS treatment.
What are the results for Spinal Cord Stimulation?
The results of Spinal Cord Stimulation (SCS) depend on careful patient selection, successful trial stimulation, proper surgical technique, and patient education. According to Mayfield Clinic, Stimulation does not cure the condition that is causing pain. Rather, it helps patients manage the pain. SCS is considered successful if pain is reduced by at least half.
Published studies of Spinal Cord Stimulation show good to excellent long-term relief in 50 to 80% of patients suffering from chronic pain [1-6]. One study reports that 24% of patients improved sufficiently to return to gainful employment or housework with stimulation alone or with the addition of occasional oral pain medication [7].
Spinal cord stimulation (SCS) therapy is reversible. If a patient decides at any time to discontinue, the electrode wires and generator can all be removed.
What are the risks of Spinal Cord Stimulation (SCS)?
No medical procedures, including surgery are without risks. General complications of any surgery include bleeding, infection, blood clots, and reactions to anesthesia. Specific complications related to SCS may include:
- Undesirable changes in stimulation (can possibly be related to cellular changes in tissue around electrodes, changes in electrode position, loose electrical connections, and/or lead failure)
- Epidural hemorrhage, hematoma, infection, spinal cord compression, and/or paralysis (can be caused by placing a lead in the epidural space during a surgical procedure)
- Battery failure and/or battery leakage
- Cerebrospinal fluid leak
- Persistent pain at the electrode or stimulator site
- A pocket of clear fluid (seroma) at the implant site. Seromas usually disappear by themselves but may require a drain.
- Lead migration, which can result in changes in stimulation and reduction in pain relief
- Allergic response to implant materials
- Generator migration and/or local skin erosion
- Paralysis, weakness, clumsiness, numbness, or pain below the level of implantation
Conditions for which you might need additional surgery include movement of the lead, breakage of the lead or extension wire, or (in rare cases) mechanical failure of the device. Reasons for removal of the device include infection and failure to relieve pain. Your doctor is responsible to explain to which of these risks, or which additional risks, apply to you.
Living with a Spinal Cord Stimulator
Once the SCS has been programmed, you are sent home with instructions for regulating the stimulation by controlling the strength and the duration of each stimulation period. Your doctor may alter the pulse width, amplitude, and frequencies on follow-up visits if necessary.
The pulse generator has programmable settings:
- Frequency (rate): number of times stimulation is delivered per second. Too few pulses results in no sensation. Too many results in a washboard or bumpy effect.
- Pulse width: the area the stimulation will cover.
- Pulse amplitude: determines threshold of perception to pain.
The handheld programmer lets you turn the stimulator on and off, select programs, and adjust the strength of the stimulation. Most people are given multiple programs to achieve the best possible pain relief at any point throughout the day or during specific activities. You can use your spinal cord stimulator around the clock if necessary.
Some people feel differences in stimulation intensity depending on their position (e.g., sitting versus standing). This is caused by variations in the spread of electricity as you change positions and is normal.
Just like a cardiac pacemaker, your stimulator cannot be damaged by devices such as cellular phones, pagers, microwaves, security doors, and anti-theft sensors. Be sure to carry your Implanted Device Identification card when flying, since the device is detected at airport security gates. Department store and airport security gates or theft detectors may cause an increase or decrease in stimulation when you pass through the gate. This sensation is temporary and should not harm your system. However, as a precaution, you should turn off your system before passing through security gates.
The various SCS systems have different restrictions to their use with MRI, ultrasound, defibrillator, electrocautery, diathermy, and cardiac pacemakers. Be sure to know the limitations of your specific SCS device. Also, chiropractic manipulation may cause the lead to move. Consult your surgeon first.
The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition.
References
- Mayfield Brain & Spine. (2018, December). Spinal Cord Stimulation, SCS, Spinal cord stimulators. Retrieved February 4, 2019, from https://mayfieldclinic.com/pe-stim.htm
- Verrills P, Sinclair C, Barnard A. A review of spinal cord stimulation systems for chronic pain. J Pain Res 9:481-92, 2016
- De la cruz P, Fama C, Roth S, et al. Predictors of Spinal Cord Stimulation Success. Neuromodulation 18(7):599-602, 2015
- Grider J, Manchikanti L, Carayannopoulos A, et al. Effectiveness of Spinal Cord Stimulation in Chronic Spinal Pain: A Systematic Review. Pain Physician 19:E33-E54, 2016
- Deer TR, Skaribas IM, Haider N, et al. Effectiveness of cervical spinal cord stimulation for the management of chronic pain. Neuromodulation 17(3):265-71, 2014
- Deer TR, Mekhail N, Provenzano D, et al. The appropriate use of neurostimulation of the spinal cord and peripheral nervous system for the treatment of chronic pain and ischemic diseases: the Neuromodulation Appropriateness Consensus Committee. Neuromodulation 17(6):515-50, 2014
- Eldabe S, Buchser E, Duarte RV. Complications of Spinal Cord Stimulation and Peripheral Nerve Stimulation Techniques: A Review of the Literature. Pain Med 17(2):325-36, 2016
- Sundaraj SR, et al: Spinal cord stimulation: A seven-year audit. J Clin Neurosci 12:264-270, 2005

Medically reviewed by Corey W Hunter, MD, FIPP - Ainsworth Institute of Pain Management and Mt Sinai Hospital
Subscribe to stay up to date about the latest in Neuromodulation and SCS
